Patient Resources
Patient education, insurance information, paperwork and more: any resource you might need as a Wilmington Endocrinology patient can be found in this section of our website. Check back often for blog updates on our publications and research.
Thyroid Cancer
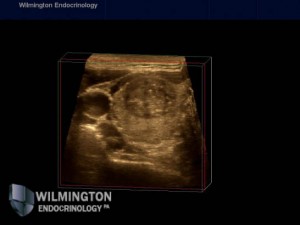
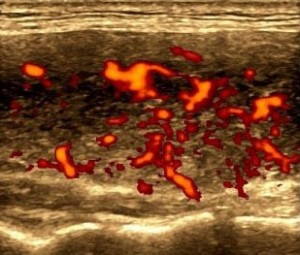
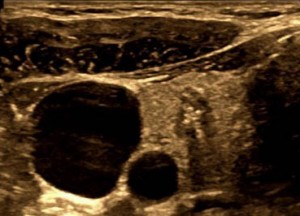 While rare compared to other cancers, thyroid cancer is the most common endocrine-related cancer. Thyroid cancer is diagnosed only after the thyroid gland is surgically removed. Thyroid cancer usually causes no symptoms. Prior to surgery, is it typical to have a Fine Needle Aspiration (FNA) biopsy to know if the nodule(s) is benign or suspicious for malignancy.
While rare compared to other cancers, thyroid cancer is the most common endocrine-related cancer. Thyroid cancer is diagnosed only after the thyroid gland is surgically removed. Thyroid cancer usually causes no symptoms. Prior to surgery, is it typical to have a Fine Needle Aspiration (FNA) biopsy to know if the nodule(s) is benign or suspicious for malignancy.
For the majority of patients, we do not know what causes them to develop thyroid cancer. However, your risk may be increased if you have history of radiation to your head or neck, a family history of thyroid cancer, or are older than 40 years of age.
The main types of thyroid cancer include: Papillary thyroid carcinoma, Follicular thyroid cancer, Medullary thyroid cancer, and Anaplastic thyroid cancer. Papillary carcinoma is the most common, making up about 80% of all thyroid carcinoma diagnosis.
 Follicular thyroid carcinoma includes follicular variant of papillary carcinoma, which is difficult to diagnose with FNA biopsy. Medullary and Anaplastic carcinomas are more rare and aggressive thyroid cancers. Thyroid cancer also runs in families, so if diagnosed, you should inform your family and encourage them to be evaluated.
Follicular thyroid carcinoma includes follicular variant of papillary carcinoma, which is difficult to diagnose with FNA biopsy. Medullary and Anaplastic carcinomas are more rare and aggressive thyroid cancers. Thyroid cancer also runs in families, so if diagnosed, you should inform your family and encourage them to be evaluated.
While the diagnosis of cancer is alarming, patients with thyroid cancer have an excellent prognosis. Thyroid cancer rarely causes pain or disability and most thyroid cancer is easily curable with surgery. After thyroid surgery and the definite diagnosis of cancer, then the plan for further treatment will be decided. Options include undergoing Radioiodine treatment or to be evaluated with serial bloodwork and neck ultrasounds.
For more information on Thyroid Cancer visit:
The Thyroid Cancer section of the Mayo Clinic Website
ATA Patient Education Brochures
Hypothyroidism
 Hypothyroidism means that you do not have enough thyroid hormone in your body. It results from having an underactive thyroid gland. It can result from autoimmune thyroiddisease, thyroid surgery, certain medications, neck radiation, or other factors. Hypothyroidism causes your body to slow down, in turn causing the following symptoms: fatigue, weight gain, cold intolerance, constipation, cold hands and feet, hair loss, brittle nails, etc. If hypothyroidism goes untreated, the signs and symptoms can gradually worsen.
Hypothyroidism means that you do not have enough thyroid hormone in your body. It results from having an underactive thyroid gland. It can result from autoimmune thyroiddisease, thyroid surgery, certain medications, neck radiation, or other factors. Hypothyroidism causes your body to slow down, in turn causing the following symptoms: fatigue, weight gain, cold intolerance, constipation, cold hands and feet, hair loss, brittle nails, etc. If hypothyroidism goes untreated, the signs and symptoms can gradually worsen.
Hypothyroidism is usually found with blood work. At our office, we typically test for TSH, free T4 and free T3. Currently, there is no cure for hypothyroidism, but in almost every patient, it can be completely controlled. The treatment for hypothyroidism is thyroid hormone replacement medication. There are many forms of thyroid hormone replacement, including, Synthroid, Levothyroxine, Cytomel, Armour Thyroid, etc.
If you are on one of these medications, it is important to take your pill first thing in the morning, an hour before eating, drinking, or taking other medications to ensure effectiveness. It is also important to have your thyroid blood levels checked 8 weeks after starting medication or having a dosage change. If you are diagnosed with hypothyroidism, you should tell your family members because thyroid disease runs in families.
For more information on Hypothyroidism:
Visit the Hypothyroidism section on the Thyroid.org website
Visit the Hypothyroidism section on the Mayo Clinic website
Hyperthyroidism
The opposite of hypothyroidism, hyperthyroidism means that you have too much thyroid hormone in your body. It results from having an overactive thyroid gland. Hyperthyroidism is usually caused by autoimmune thyroid disease, thyroid nodules, some medications, pregnancy, or other factors. Because hyperthyroidism speeds your body up, symptoms can include: fatigue, weight loss, increase in appetite, anxiety, nervousness, heat intolerance, palpitations (racing heart), increased heart rate, etc. Untreated hyperthyroidism can lead to atrial fibrillation, bone loss, and heart disease.
 Like hypothyroidism, hyperthyroidism can be confirmed with blood work. We usually test for TSH, free T4, free T3, blood count, hepatic function, and TSH receptor antibody. The TSH receptor antibody is the antibody for Grave’s disease. Grave’s disease is autoimmune hyperthyroidism. Short-term treatment of hyperthyroidism includes antithyroid medications such as PTU and Methimazole.
Like hypothyroidism, hyperthyroidism can be confirmed with blood work. We usually test for TSH, free T4, free T3, blood count, hepatic function, and TSH receptor antibody. The TSH receptor antibody is the antibody for Grave’s disease. Grave’s disease is autoimmune hyperthyroidism. Short-term treatment of hyperthyroidism includes antithyroid medications such as PTU and Methimazole.
Once your levels have normalized, there are more permanent treatment options such as Radioiodine treatment and surgery to have your thyroid gland removed. These two procedures will leave the patient with hypothyroidism. About 20-30% of patients can develop remission. This means their thyroid gland can normalize and the antithyroid medication can be stopped. These patients are at risk for relapse. If you are diagnosed with hyperthyroidism, you should tell your family members because thyroid disease runs in families.
For more information on Hyperthyroidism:
Visit the Hyperthyroidism section on Thyroid.org website
Visit the Hyperthyroidism section on the Mayo Clinic website
Hashimoto’s Disease
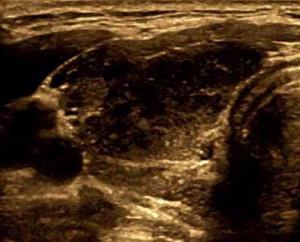
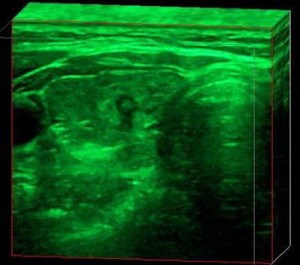
 Hashimoto’s disease, also known as chronic lymphocytic thyroiditis, is an autoimmune disease where the body’s immune system attacks the thyroid gland. This attack on the gland can lead to inflammation and ultimately, the gland not working appropriately (hypothyroidism). This inflammation can also lead to thyroid nodule formation. As with other thyroid diseases, our office can diagnosis Hashimoto’s disease with blood work. The blood work for Hashimoto’s is TSH, free T3, free T4, thyroidperoxidase antibody and antithyroglobulin antibody.
Hashimoto’s disease, also known as chronic lymphocytic thyroiditis, is an autoimmune disease where the body’s immune system attacks the thyroid gland. This attack on the gland can lead to inflammation and ultimately, the gland not working appropriately (hypothyroidism). This inflammation can also lead to thyroid nodule formation. As with other thyroid diseases, our office can diagnosis Hashimoto’s disease with blood work. The blood work for Hashimoto’s is TSH, free T3, free T4, thyroidperoxidase antibody and antithyroglobulin antibody.
There is no real treatment for Hashimoto’s thyroiditis, but once your thyroid hormone levels are affected, then you can be started on thyroid hormone replacement. Hashimoto’s also runs in families. In our recent study on 2,500 patients with thyroid nodules, we examined the relationship between autoimmune thyroid disease and cancer. We found that patients with autoimmune thyroid disease may be at higher risk for thyroid cancer. Specifically, elevated antithyroglubulin antibody level was an independent risk factor for thyroid malignancy.
For more information on Hashimoto’s Disease:
Visit the Hashimoto’s Disease section on the Mayo Clinic website
Other Endocrine Disorders
For more information on other Endocrine disorders, please see the links below.
Diabetes
Diabetes.org
Minimed.com
Gestational Diabetes
Polycystic Ovary Syndrome
Pituitary
Pituitary Society
Pituitary Network Association
Osteoperosis
Parathyroid
Hyperparathyroidism
Hypoparathyroidism


